Case Studies
| |
The following case studies were conducted at various hospitals throughout Southern California and implemented a standardized testing procedure to insure accuracy of the results.
Most studies were performed by registered nurses belonging to the Wound Ostomy and Continence Nurses Society, an organization promoting the advancement of health care with an emphasis on skin care relating to abdominal stomas, wounds, fistulas, drainage, pressure sores and incontience.
We have included these studies hoping to give you some insight as to possible applications and performance of Calmoseptine® Ointment.
Some of the images contained within this section may not be suitable for children under the age of 18. Graphic images displayed are wounds and areas of irritation including but not limited to the rectum and buttocks, female and male genitals, and stomal sites. Please proceed with caution.
| |
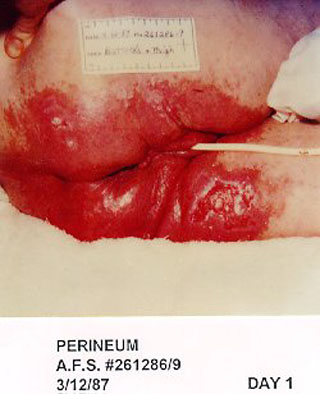
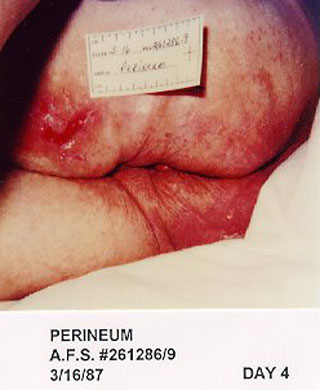
85 year old female with sepsis and dehydration.
Investigator: Mickey Foreman, RNET
Facility: San Gabriel Valley Medical Center, San Gabriel, CA
Patient Code: A.F.S. # 261286-9
Date of Case Study: 3/12/87 - 3/16/87
The patient is an 85 year old female admitted to an acute care facility with sepsis and dehydration. She was incontinent of constant liquid stools causing severe, denuded buttocks with serous, bloody exudation. This area measured 12" x 12". She also had a stage III dermal ulcer on her right thigh measuring 5 cm x 5 cm. Calmoseptine® Ointment was applied four times daily and the buttocks were totally pain free and healed within four days. The ulcer healed to a stage II and was half the original size.
81 year old female with multiple decubiti and debilitation.
65 year old male with bowel obstruction and history of prostatic carcinoma
Investigator: Odette Hammond, RNET
Facility: Hollywood Presbyterian Medical Center, Los Angeles, CA
Patient Code: #00305573
Date of Case Study: 2/1/88 - 2/4/88
The patient is an 81 year old female admitted to an acute care facility with multiple decubiti and debilitation. This patient had 8-10 loose stools in 24 hours. Severe, painful excoriation occurred involving an area of the perineum measuring 8 x 10 inches. Calmoseptine® Ointment was applied twice daily and 3 days later the area was healed to a small remaining pink area 1 x 3 inches.
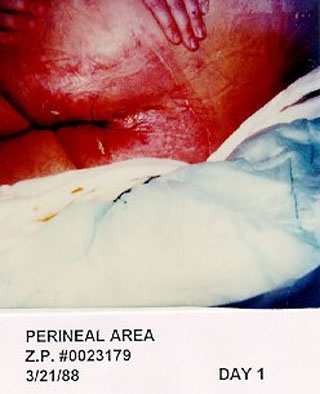
Investigator: Renee Kalkbrenner, RNET, BSN
Facility: Huntington Memorial Hospital, Pasadena, CA
Patient Code: Z.P. #0023179
Date of Case Study: 3/21/88 -3/28/88
The patient is a 65-year-old male who was admitted to Huntington Memorial Hospital with a bowel obstruction and a history of prostatic carcinoma. He developed a stage III pressure ulcer and underwent radiation therapy for his cancer. This patient had 6 fecal incontinent episodes daily. A painful, reddened area measuring 24 cm x 24 cm around the sacral area was caused by this incontinence. The area also had a scant amount of serous drainage. Calmoseptine® Ointment was applied 3 times daily and the area was much improved in 5 days and the patient was pain free. The area of redness was totally resolved in 7 days. The pressure ulcer, remaining resistant to all other modalities of therapy, required plastic surgery.
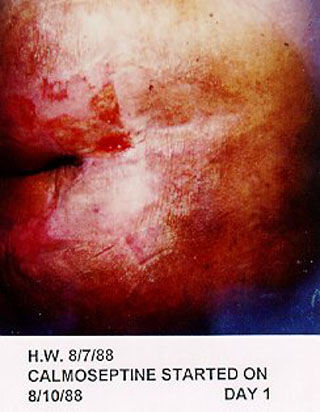
89 year old female with fecal and urinary incontinence
Investigator: Mary Beaty, RNET
Facility: Pomona Community Hospital, Pomona, CA
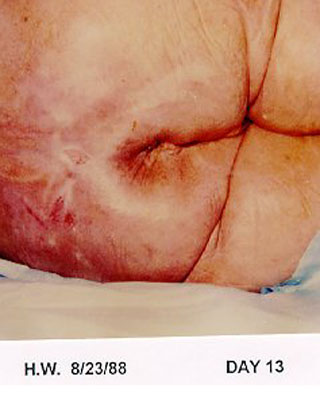
Patient Code: H.W.
Date of Case Study: 8/7/88 - 8/23/88
The patient is an 89 year old female admitted to an acute care facility with necrotic feet. She had two amputations; one above the knee on the left leg and one below the knee on the right leg. Her age and immobility were contributing factors to her deteriorating condition. She had continuous fecal and urinary incontinence. The excoriated area also developed a stage II draining pressure ulcer and was extremely painful. The total affected skin area was 8" x 8". Calmoseptine® was applied 3-4 times daily to the perineal area. The area was healed within 13 days. Pain was relieved within 2 days of application.
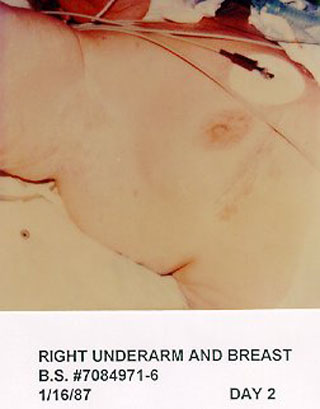
69 year old male with gunshot wound, urinary incontinence, painful redness
Investigator: Mary Beaty, RNET
Facility: Pomona Community Hospital, Pomona, CA
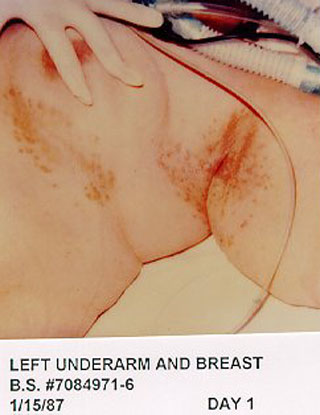
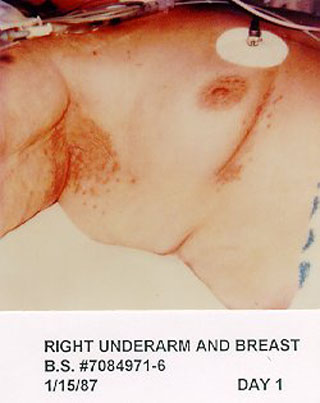
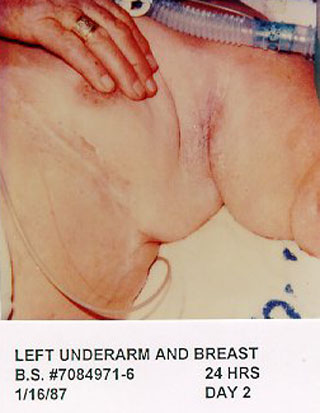
Patient Code: B.S. #7084971-6
Date of Case Study: 1/15/87 - 1/16/87
The patient is an elderly female with a combination of the following diagnoses: diabetes mellitus, acute M. I., renal failure, respiratory failure and she also had cardiac bypass surgery. She developed a yeast infection in the skin fold areas of her under arm measuring 4" x 4" and under her breast measuring 2" x 6". Calmoseptine® Ointment was applied twice daily and the area was completely healed in 24 hours.
Elderly female with yeast infection in skin fold
Investigator: Barbara McBride-Schuck, RNET
Facility: Methodist Hospital of Southern California, Arcadia, CA
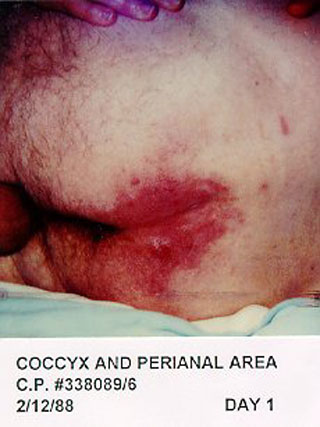
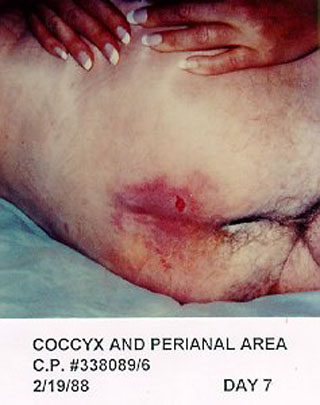
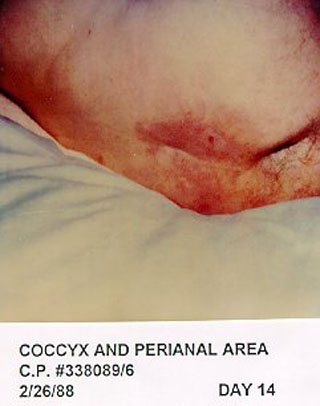
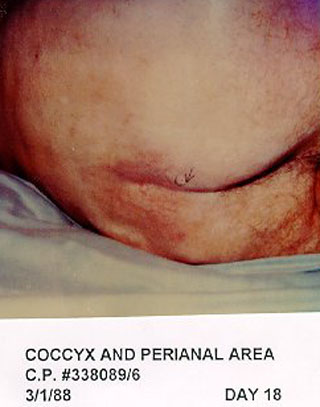
Patient Code: C.B. #338089-6
Date of Case Study: 2/12/88 - 3/1/88
The patient is a 69 year old male with a gunshot wound requiring multiple surgeries. He was incontinent of urine, which was treated by diapering the area. This patient developed an area of painful redness 12 cm x 7 cm x .75 cm. Calmoseptine® Ointment was applied four times daily. Gradually the area was completely healed from pain relief in 19 days.
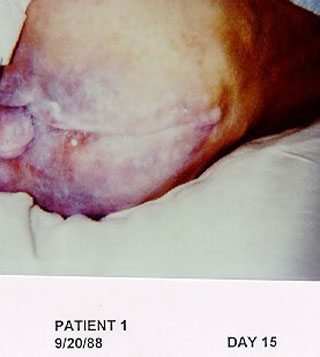
67 year old with diaper rash on perirectal and scrotal areas
Investigator: Janet Ursua RNET
Facility: San Antonio Community
Hospital
Patient Code: Patient 1
Date of Case Study: 9/5/88 - 9/20/88
The patient is a 67 year old male admitted with uncontrolled diabetes and diarrhea. The patient had a poor attitude about himself and had a lack of interest in his care, which were contributing factors to his outcome. He was incontinent of liquid stool 10-12 times in 24 hours and was previously managed by diapering. He developed an extremely painful area that was excessively bloody, red and macerated on his perirectal and scrotal areas measuring 24 cm x 20 cm. Calmoseptine® Ointment was applied Q.I.D. and the pain, maceration and exudation were completely resolved by the 15th day of treatment. The remaining perirectal area was slightly pink measuring 19 cm x 16 cm.
85 year with female fecal and urinary incontinence
Investigator: Ann Marie Knudsen, RNET
Facility: Hospital Home Health Care Agency of California, Torrance, CA
Patient Code: # 0089214
Date of Study: 4/12/89 - 4/26/89
The patient is an 85 year old female seen in her home. The patient has continuous fecal and urinary incontinence. Her age and lack of appropriate hygiene are the contributing factors to the excoriated skin on her coccyx and perianal area. She had developed a severe, painful excoriation measuring 15 cm x 7 cm on her buttock continuing between her legs. Patient is wearing disposable diapers. Good hygiene was demonstrated and Calmoseptine® Ointment was applied daily after a sitz bath. After three days, the patient was pleased with the relief from pain and burning that she meticulously continued the treatment daily and after 12 days her skin had completely healed. Patient is continuing using Calmoseptine® Ointment daily as prevention of further skin damage.
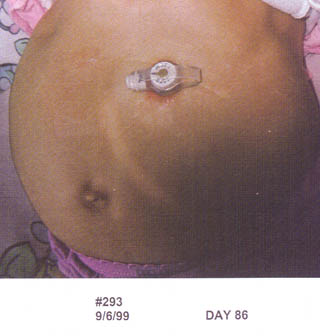
4 year old with excoriation of skin around gastrostomy tube
Investigator: Melanie Kingsbury RN
Facility: Morning Star Home Health Care
Patient Code: # 293
Date of Study: 6/12/99 - 9/6/99
The patient was a 4 year old with chronic respiratory failure and Jeune's syndrome with Thoracic Dystrophy. The patient also had a tracheostomy and was partially ventilator dependent. A gastrostomy tube was in place for feedings. Feeding tube site leakage was chronic causing constant excoriation of the skin around the tube. The painful excoriation measured approximately 3/8 inch around the tube. Previous methods of management included nystatin powder, bacitracin, and A&D ointment. Calmoseptine® Ointment was applied twice daily starting on 6/12/99 and covered with a small piece of gauze (after cleansing gently with mild cleanser and water). The patient was pain free by 6/19/99 and the lower edge of the skin was healed by 6/26/99. The skin continued to improve until total healing was achieved by 9/6/99.
38 year old with urinary peristomal erosion
Investigator: Terry Crawford, RNET
Facility: Queen of the Valley Hospital Home Care, Napa, CA
Patient Code: M.D.
Date of Study: 6/8/99 - 10/5/99
The patient was a 38 year old quadriplegic with a one-year history of urinary peristomal erosion. This erosion started out to be less than 1 cm and kept enlarging until it was 11 cm x 10.5 cm with a second wound inferior to the peristomal wound. Previous methods of management included the use of an appliance, Iodoflex and Calcium Alginate without success.
The urostomy appliance was discontinued on 6/8/99, a 22 Fr Foley Catheter was inserted into the stoma and secured with Montgomery straps. Calmoseptine® Ointment was applied to the wound and peristomal area once daily and covered with a dry dressing. There was much improvement within one month and the area was totally healed by 10/5/99. The patient was also pain free.
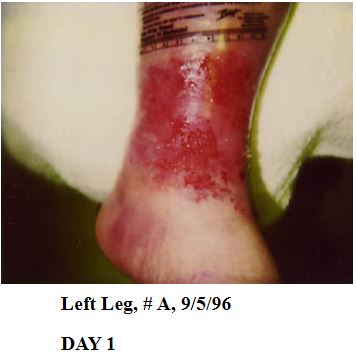
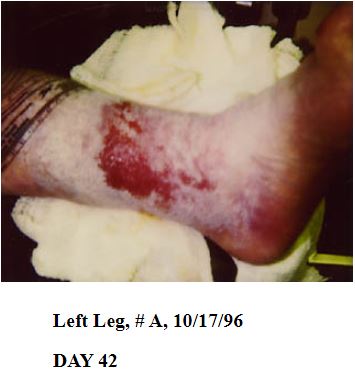
56 year old with superficial ulcer of the left lower leg
Investigator: Viola Lias Conover
Facility: St. Lukes Medical Center
Patient Code: # A
Date of Study: 10/3/96 - 1/16/97
The patient is a 56 year old male with venous insufficiency. Both lower legs were weepy and edematous. The pitting edema varied from day to day. He developed a superficial ulcer of the left lower leg measuring 9.2 cm x 9.3 cm, which drained serous to serosanguineous drainage. The ulcer was painful when cleansed or touched. There was also intense itching sensations to the legs. For 6 months, several different treatments failed to heal the ulcer. On 10/10/96 treatment was started by first cleansing the lower leg with whirlsol solution and then applying Calmoseptine® Ointment to the wound on a 4x4 gauze daily. The lower leg was then wrapped in tubigrip for compression. By 1/16/97 the ulcer was healed. Itching is also relieved when Calmoseptine® Ointment is used. When treatment is stopped the patient's ulcer recurs along with the itching. He is now maintained for 1-1/2 years with this treatment and the ulcer remains healed.
48 year old with superficial venous stasis ulcer
Investigator: Viola Lias Conover
Facility: St. Lukes Medical Center
Patient Code: # B
Date of Study: 7/96 - 10/98
The patient was a 48 year old with hypothyroidism, chronic venous insufficiency and a superficial left medial ankle venous stasis ulcer measuring 3 cm x 4 cm. There was also peri-wound skin irritation and heavy perspiration. The area was weepy and very erythematous with mild pain. This patient was very active in biking and walking several miles per day.
From 7/96-12/96, unsuccessful methods of management were foam dressing, unna boot and a hydrocolloid. The treatment was changed on 12/13/96 to daily dressing changes with Calmoseptine® Ointment saturated 4x4's to the ulcer. Sween Cream was applied to the dry peri-wound skin. The ankle was wrapped with kerlix wrap and a light compression device (Jobs), was applied. The area was healed by 8/15/97. It was noted that when this treatment was discontinued the area would begin to breakdown within one month. The area remains healed as of 2/19/99.